COVID-19 pandemic personal protective equipment (PPE): Guidance for intensive care
31 July 2020
Summary
Infection Prevention & Control (IPC) guidance is developed on the best evidence available at any given time. It is for individual organisations to determine how best to implement it in order to protect their staff & patients.
These guidelines are written in support of critical care delivery and offer a pragmatic interpretation of the current generic PHE guideline.
These guidelines should be read in conjunction with:
https://icmanaesthesiacovid-19.org/clarification-of-ppe-guidance-during-planned-surgery-restarts
The above documents provide a framework for local risk assessment based upon community transmission of COVID-19.
National and local policy on the safe delivery of care is changing frequently as lockdown relaxes and more targeted local interventions are introduced. Local risk assessment processes should be applied when interpreting guidance.
The critical care community must plan for the continuing provision of critical care services in the context of variable ongoing community transmission of the SARS-CoV-2 virus and the potential for further waves.
In addition to providing COVID-19 facing critical care capacity, there is a rise in demand for critical care for patients with non-COVID-19 illness.
The need for parallel streams of clinical care for COVID-19 positive and COVID-19 negative is placing a considerable demand on the ICU.
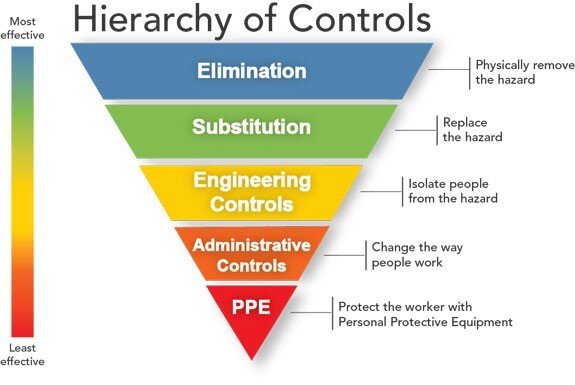
Minimising occupational transmission of COVID-19 infection to healthcare workers and nosocomial transmission of COVID-19 to patients, will require a combination of approaches.
The risk of transmission of the SARS-CoV-2 virus in this clinical area is related to contact with respiratory droplets and aerosols generated by the patient during clinical care and by fomite contamination of the clinical environment with persistence of viable virus.
Standard infection control measures must be applied and PPE must be appropriate: https://www.hse.gov.uk/coronavirus/assets/docs/face-mask-equivalence-aprons-gown-eye-protection.pdf and based upon transmission.
We advocate an approach which allows those who personally feel they prefer additional PPE to be provided with this and supported in its use. This should be influenced by individual risk assessments.
Summary of PPE guidance
Summary of PPE guidance
|
Non COVID-19 patients |
Non AGP |
AGPs |
|
Elective |
Standard infection control precautions |
|
|
Fluid resistant surgical facemask |
||
|
Gloves and apron, for direct contact with blood and body fluids only – change between tasks and patients |
||
|
Eye protection if risk of splashing of body fluid |
||
|
No need to use side rooms |
||
|
Emergency |
Non AGP |
AGPs |
|
Standard infection control precautions |
||
|
Fluid resistant surgical facemask |
||
|
Eye protection if risk of splashing of body fluid |
||
|
Gloves and apron** for direct contact with blood and body fluids only – change between tasks and patients |
Gloves and apron**, within 2m of patient– change between tasks and patients |
|
|
|
*Use of side rooms for AGPs |
|
|
Enhanced environmental cleaning |
||
*Local decisions around placement in non COVID-19 areas will have been made by senior clinical staff in conjunction with local guidance, and take into account the risk/benefit balance based on clinical presentation, COVID-19 contact history, imaging results, COVID-19 prevalence and the nature and number of negative PCR samples. Routine use of side rooms for AGP in patients considered low risk is likely to be impractical in most units due to low numbers of side rooms.
**Gloves and aprons must be removed and hands decontaminated immediately after the episode of care and before touching shared equipment such as computers, phones or desk surfaces.
|
Suspected or proven COVID-19 |
Single patient – no AGP |
Single patient - AGP |
Patients - AGPs in cohorted areas |
|
Sessional use |
FRSM mask |
FFP3 mask |
FFP3 mask |
|
Eye protection if risk of splashing of body fluid |
Eye Protection |
Eye protection |
|
|
|
Gown* |
Gown* |
|
|
Change between patients and tasks |
Gloves** for direct contact with the patient or their environment |
Gloves** for direct contact with the patient or their environment |
Gloves for direct contact with the patient or their environment |
|
Plastic apron** |
|||
|
Patient location |
Side room (if possible but prioritise for COVID-19 patients undergoing AGP) |
Use side room |
Designated areas in ICU with physical barrier |
|
Enhanced Environmental Cleaning |
|||
* Gowns should be water repellent or protected with a plastic apron if there is a risk of splashing of body fluid. The same gown should not be used to care for more than one patient. If this is not possible, the gown must be protected with a plastic apron and changed between patients. Short sleeved gowns enable hands and arms to be to be washed and therefore minimise the risk of cross transmission.
**Gloves and aprons must be removed and hands decontaminated immediately after the episode of care and before touching shared equipment such as computers, phones or desk surfaces
Note: it is essential to apply Standard Infection Control Precautions in the care of all patients.
COVID-19 risk assessment and clinical pathways
All critically ill patients admitted to the ICU should be assessed for their risk of COVID-19 infection. Local and regional incidence data will help inform this decision. With the increased availability and capacity of SARS-CoV-2 PCR testing, the infection status of many patients will be known on admission to ICU, or shortly thereafter.
Elective patients
Current guidance should be followed re quarantine and screening.
Where this has not been possible local consideration could be given to managing this patient group as emergency patients.
Current guidance re repeat testing should be followed.
In the event that a patient develops an acute febrile illness of uncertain aetiology in the post-operative period, the possibility of COVID-19 infection should be considered.
Emergency patients:
These patients may be deemed:
at low risk of COVID-19 infection by virtue of low community transmission rates and/or the nature of the presenting illness and/or a negative PCR SARS-CoV-2 test on naso-pharyngeal swab or lower respiratory tract samples
suspected of COVID -19 infection by virtue of the nature of the presenting illness (and are awaiting SARS-CoV-2 PCR testing) or are test negative but still remain clinically suspicious
positive for COVID-19 infection on the basis of clinical symptoms and positive SARS-CoV-2 PCR testing
Previously confirmed COVID-19 infection, but no longer considered an infection risk.
Principles:
Patients no longer infectious 14 days after onset of symptoms
Period of infectivity may be longer in patients who are severely ill
A positive PCR test does not indicate infectivity as the genome continues to be excreted from dead cells for weeks after the infection has been cleared (see figure)
Sethuraman et al JAMA April 2020
Recommendation (see Appendix 1)
Isolation precautions for COVID-19 patients on or after Critical Care Unit admission are discontinued if the following conditions are met.
14 days have elapsed since first positive SARS-CoV-2 test AND there has been:
sustained clinical improvement with at least some respiratory recovery
absence of fever (> 37.8°C) for 48 hours
no underlying severe immunosuppression
one negative SARS-CoV-2 tests taken on day 14 from the lower respiratory tract (or upper respiratory tract if lower not possible)
if still positive on day 14, a further sample should be tested at 7-day intervals until a negative swab.
On occasion, critically ill patients recovering from COVID-19 infection may continue to demonstrate SARS-CoV-2 PCR positivity on serial testing for many weeks. This does not necessarily reflect the presence of viable virus nor the ability to transmit infection. In the absence of underlying severe immunosuppression, ICU clinicians should liaise with local infection experts (microbiology, infectious diseases) to agree when isolation precautions may be reasonably relaxed in such circumstances.
ICU preparedness for the prevention and control of COVID-19 infection
To deliver Critical Care through different phases of pandemic, local ICU escalation policies should:
Identify the location of areas
Identify the number of beds
Identify the IPC measured required at each step of ICU escalation for patients with proven or highly suspected COVID-19
Intensive care services have developed plans and processes for dealing with patients with both COVID-19 infection and non-COVID critical illness. The principles and practice of running parallel streams of critical care provision are now well established.
The use of colour descriptors to identify the nature of critical care beds has become widespread and is often integrated with Trust-wide policies. There is no nationally accepted process for this colour allocation - so care should be taken when interpreting guidance from elsewhere.
Within Critical Care standardisation would be beneficial, we suggest:
Green for non COVID-19 patients, Amber for suspected COVID-19 (clinically suspicious and awaiting test or high index of suspicion) and Blue for COVID-19 positive patients
Individual ICU design and side room availability will dictate how these pathways are managed.
All of the elements of the hierarchy of IPC measures must be considered
https://www.cdc.gov/niosh/topics/hierarchy/
Standard infection prevention and control measures must be adhered to.
The form of PPE worn by staff should be commensurate with the risk to the healthcare worker of acquiring COVID-19 infection and should be informed by, community transmission the nature of the ICU clinical area and patient characteristics.
At the start of the pandemic, all ICUs were considered high risk areas, there is an opportunity now to consider that only critical care areas which cohort suspected/proven cases of COVID-19 or those areas admitting emergency patients for additional risk assessment/testing should be regarded as high risk areas, this must be done by local risk assessment based upon:
Community transmission
The number of COVID-19 patients within critical care units and hospital
Availability of rapid testing
Estates ability to provide COVID-19 negative areas
Aerosol generating procedures (AGP)
These are defined by PHE https://www.gov.uk/government/publications/wuhan-novel-coronavirus-infection-prevention-and-control/covid-19-personal-protective-equipment-ppe
Continued review of the evidence base for Aerosol Generating Procedures by NERVTAG is imperative, in a practical sense there is a difference between close proximity, time limited AGPs (intubation, tracheostomy insertion, open suctioning of tracheostomies ) and continued low level, low droplet / aerosol dispersal procedures such as Nasal High Flow Oxygen and CPAP use. This impacts heavily on the practicalities of PPE use.
The non-COVID ICU
General Principles
It is recognised that it is neither practicable nor necessary to wear Airborne PPE in the lower risk area of the non-COVID ICU. Not only is this clinical practice potentially wasteful of a precious resource but the infection prevention and control implications of wearing this style of PPE whilst caring for a heterogenous critically ill population may be considerable and could give rise to an increased risk in healthcare associated infection.
The organisational control measures will serve to reduce the risk of COVID-19 infection arising in staff or patients working in the non-COVID ICU.
The universal wearing of FRSMs in the clinical environment combined with good respiratory hygiene and frequent hand washing is designed to reduce the risk of inadvertent transmission of coronavirus infection from asymptomatic individuals.
Infection control principles & PPE
Currently all staff entering the clinical environment of the non-COVID ICU should wear a FRSM in keeping with national guidelines.
The principles of social distancing should be adhered to wherever practicable.
Standard infection-control procedures should be adhered to by all staff in the ICU
Elective
Patients in the Green Elective patient group are neither suspected or confirmed COVID-19, and could therefore be considered to be low risk (dependent upon local risk assessment), the following minimal PPE is appropriate
|
Non AGP |
AGPs |
|
Standard infection control precautions |
Standard infection control precautions |
|
Fluid Resistant Surgical Facemask |
Fluid Resistant Surgical Facemask |
|
Gloves and apron for direct contact with blood and body fluids only – change between tasks and patients |
|
|
Eye protection if risk of splashing of body fluid |
|
|
No need for side rooms |
No need to use side rooms |
Emergency
Patients in the non-COVID-19 Emergency patient group (i.e. low clinical index of suspicion, ix naso pharyngeal swab) are neither suspected or confirmed COVID-19 but with sustained community transmission continue to present a slightly increased risk above those in the Elective group. A negative lower respiratory tract sample for SARS-CoV-2 PCR has improved negative predictive value and provides increased confidence for decision making.
In areas of low community prevalence, the risk probably approaches that of the elective group, local policy should inform local PPE guidance based upon risk assessment.
|
Non AGP |
AGPs |
|
Standard infection control precautions |
|
|
Fluid resistant surgical facemask |
|
|
Eye protection if risk of splashing of body fluid |
|
|
Gloves and apron for direct contact with blood and body fluids only – change between tasks and patients |
Gloves and apron, within 2m of patient – change between tasks and patients |
|
|
*Use of Side rooms for AGPs |
|
Enhanced environmental cleaning |
|
*Local decisions around placement in non COVID-19 areas will have been made by senior medical staff in conjunction with local guidance, and take into account the risk/benefit balance based on clinical presentation, COVID-19 contact history, imaging results, COVID-19 prevalence and the nature and number of negative PCR samples. Routine use of side rooms for AGP in patients considered low risk is likely to be impractical in most units due to low numbers of side rooms.
COVID-19 suspected or positive patients in ICU
General Principles
A clinical area should be designated as the COVID-ICU. This area should be large enough to meet the anticipated clinical demand.
Side-rooms (negative pressure if available) should be utilised for the admission of suspected cases of COVID-19 infection in whom test results are awaited.
Confirmed cases may be cohorted together.
Cohorting of suspected and confirmed cases of COVID-19 infection should be avoided where possible.
In patients with high clinical index of suspicion of COVID-19 who have a negative nasopharyngeal swab PCR on admission, re-testing in the following 12-24 hours is appropriate, obtaining a deep respiratory sample whenever possible. These patients should ideally, be cared for in side rooms, until their COVID-19 status is determined
As numbers of COVID-19 positive patients fall significantly within critical care units, it may me more practicable, where possible to care for them on a “normal” ICU, isolating these patients in side rooms, with appropriate areas for “donning and doffing” PPE. The doffing process (with the exception of the mask) should happen either prior to exiting the side room itself, or in the anteroom if present. The mask should then be removed having exited the room. Healthcare Workers should not be exiting the room wearing PPE.
When undertaking sterile procedures, existing gowns and gloves should be doffed, hands washed in the normal manner prior to a sterile procedure and a new set of sterile gloves and gown utilised.
Nursing staff should be dedicated to the care of a suspected COVID-19 patient and should not be assisting in the care of confirmed COVID-19 patients during the same clinical session.
Medical staff should prioritise the clinical review of COVID-19 suspected patients on a ward-round before seeing those with confirmed infection.
Infection control principles & PPE for COVID-19 suspected or positive patients
Appropriate infection-control procedures must be adhered to by all staff in the ICU, including standard infection control principles.
Healthcare workers should wear appropriate PPE commensurate with the risk of transmission of COVID-19 infection
The risk of transmission of the SARS-CoV-2 virus in this clinical area is related to contact with respiratory droplets and aerosols generated by the patient during clinical care and by fomite contamination of the clinical environment with persistence of viable virus.
|
Suspected or proven COVID -19 |
Single Patient – no AGP |
Single patient - AGP |
Patients with AGPs in cohorted areas |
|
Sessional use |
FRSM mask |
FFP3 mask |
FFP3 mask |
|
Eye protection if risk of splashing of body fluid |
Eye Protection |
Eye protection |
|
|
|
Gown* |
Gown* |
|
|
Change between patients and tasks |
Gloves** for direct contact with the patient or their environment. |
Gloves** for direct contact with the patient or their environment. |
Gloves - for direct contact with the patient or their environment. |
|
Plastic apron** |
Plastic apron** |
Plastic apron** |
|
|
Patient location |
Side Room (if possible but prioritse for COVID patients undergoing AGP) |
Use Side room |
Designated areas in ICU with physical barrier |
|
Enhanced environmental cleaning |
|||
*Gowns should be water repellent or protected with a plastic apron if there is a risk of splashing of body fluid. The same gown should not be used to care for more than one patient. If this is not possible the gown must be protected with a plastic apron and changed between patients. Short sleeved gowns (although not currently widely available) do enable hands and arms to be to be washed and therefore minimise the risk of cross transmission.
**Gloves and aprons must be removed, and hands decontaminated immediately after the episode of care and before touching shared equipment such as computers, phones or desk surfaces.
Note: it is essential to apply standard infection control precautions in the care of all patients
Ensuring infection prevention and control when cohorting COVID-19 patients
Whilst delivering clinical care within the COVID-ICU, there is a significant risk of cross-infection. This is an inherent problem with the nature of the Airborne PPE, which is required to be worn in order to prevent transmission of COVID-19 infection to the health care worker. The risk of cross infection requires specific mitigation by staff providing care to multiple patients in a single clinical session.
Gloves are only required for direct contact with the patient or their immediate environment and must be changed between tasks on the same patient and between patients. They must not be worn to touch shared equipment such as computers, phones or desk surfaces.
COVID-19 is transmitted via the mucus membranes (eyes, nose and mouth), there is no reason for continual glove use and hand hygiene is best practice.
Whilst providing personal care or examining a patient, staff should wear a disposable plastic apron over the sessional use gown and change this between patients.
The apron can be donned by breaking the neck loop with a buddy re-tying the torn ends around the neck of their colleague. Following the clinical interaction, the plastic apron should be removed and discarded along with the gloves and hand hygiene performed.
If sessional use gowns are long sleeved, then there is still a risk that pathogens will be transferred between patients on the sleeves.
Recommendations for avoiding transmission of pathogens between patients when cohorting COVID-19 patients
The following principles aim to minimise the risk of pathogens being transferred on PPE that comes into direct contact with the patient.
1. Gloves
Healthcare workers should wear a single pair of gloves which must be removed following delivery of each episode of clinical care and between different tasks on the same patient within the cohorted ICU area.
The gloves should be discarded following removal and then hands are washed with soap and water or alcohol hand gel/rub as per standard clinical practice. Once hand hygiene has been performed and the hands dried, a fresh pair of gloves could be donned.
Although this requires the healthcare worker to remove their protective gloves and decontaminate their hands in the clinical area, removing gloves in the clinical area does not present a risk to the healthcare worker because the virus does not cause infection via the skin.
If wearing a long sleeved gown it may be difficult to avoid wetting the arms if washing hands with soap and water. This can be avoided by using alcohol hand gel to decontaminate hands (this is perfectly acceptable given that hands have been protected with gloves and will therefore not be soiled.). Additionally, the cuffs can be pulled up the arms away from the hands to perform hand hygiene.
2. Gowns and aprons
Wherever possible the same gown must not be used to care for more than one patient. If this is not possible then the following good practice must be applied to minimise the risk of transmission of pathogens between patients:
Protect the gown with disposable waterproof arm sleeve covers with elasticated cuffs and a plastic apron. Following each episode of clinical care with a patient in the cohorted ICU area both the apron and the disposable arm sleeve covers must be removed and discarded. Gloves must also be removed between tasks on the same patient (as pathogens may be introduced to susceptible sites and cause infection). The hands must be washed with soap and water or decontaminated with alcohol gel. Once hand hygiene has been performed a pair of fresh gloves in combination with disposable arm sleeve covers could be donned.
Protect the sleeves of the gown with long cuffed disposable gloves. These must be removed between patients and between tasks on the same patient. A plastic apron should be used to protect the amin body of the gown and changed between patients.
The Healthcare worker wears a specifically designed short sleeved gown to cover their surgical scrubs which may be re-processed by laundering. During patient care episodes (within 2m) they wear a disposable apron (which could be long sleeved) and gloves.
This allows the forearms and hands to be washed between patient contact episodes. Remaining sessional PPE protects the healthcare worker against COVID-19 in the general cohort areas, including self-contamination. If a standard apron does not provide sufficient cover to the upper arms, a long sleeved disposable apron should be used.
Using a long-sleeved apron in combination with a short sleeved sessional gown appears to provide the best solution to this problem.
The following practices are NOT recommended for managing patients with COVID-19.
Double gloving, there is no evidence that decontaminating gloves in clinical settings is effective at providing an adequate level of hand hygiene. https://www.who.int/gpsc/5may/Glove_Use_Information_Leaflet.pdf
The clinical practice of “double gloving” is not required and does not provide the healthcare worker with enhanced protection from the SARS-COV-2 coronavirus.
Alcohol gelling gloves (rather than hand washing), there is no evidence that gelling gloves between patients is effective in clinical areas.
Hair coverings are not required, although we recognise that individuals may prefer to wear them, there is no evidence that hair acts as a route of transmission or that hair covering makes any contribution to preventing transmission.
Fluid repellent coveralls are not essential to protect Healthcare Workers from COVID-19 which is transmitted by respiratory droplets. Guidelines allow for their use however, whilst providing a good level of protection they are challenging to wear for long periods of clinical duty. In addition, the doffing of fluid repellant coveralls is a more complex process which requires practice by healthcare workers before attempting to use in the clinical environment.
References
https://icmanaesthesiacovid-19.org/clarification-of-ppe-guidance-during-planned-surgery-restarts
https://www.hse.gov.uk/coronavirus/ppe-face-masks/health-social-care/index.htm
Klompas M, Baker MA, Rhee C. Airborne Transmission of SARS-CoV-2: Theoretical Considerations and Available Evidence. JAMA. Published online July 13, 2020. doi:10.1001/jama.2020.12458
Estimating the risk of an anaesthetist acquiring COVID-19 by anaesthetising an asymptomatic patient, July 6, 2020 Letter https://doi.org/10.1177/0310057X20937316
https://bjanaesthesia.org/article/S0007-0912(20)30213-0/fulltex
https://www.who.int/gpsc/5may/Glove_Use_Information_Leaflet.pdf
https://www.cdc.gov/niosh/topics/hierarchy/
Appendix 1 - Underpinning Guidance
Public Health England inpatient step-down of infection prevention and control (IPC) in hospitalised patients with COVID-19.
(Guidance on step-down 23rd April 2020)
Continue IPC measures until 14 days have elapsed since their first positive SARS-CoV-2 test.
IPC measures for hospitalised COVID-19 patients can be stopped if there is:
clinical improvement with at least some respiratory recovery
absence of fever (> 37.8°C) for 48 hours
no underlying severe immunosuppression
Consider testing at day 14 since first positive SARS-CoV-2 test (lower respiratory tract sample if the patient is producing sputum or is intubated). One negative test is acceptable for step-down
ENDS